Bringing mental health resources to the frontlines of care with technology
As levels of stress, anxiety and depression have risen among healthcare workers throughout the Covid-19 pandemic, frontline community health agents in Brazil are using a new app to prioritise their resilience and wellbeing
Ever since the World Health Organization (WHO) declared the coronavirus outbreak to be a pandemic, on March 11 2020, the virus has had a profound effect on the social and economic changes on people's daily lives and on their mental health and wellbeing in particular.
As early as March 18 2020 the WHO acknowledged the potential impact of the pandemic on the mental health of the general population, stating that it had the potential to become a public health emergency.
Since then, research from countries such as the UK, China and Australia has shown sharp and widespread increases in rates of anxiety and depression, while frontline healthcare workers appear to have been affected disproportionately — including those in Brazil, where a recent study has shown that rates of mental health disorders are above 30 per cent.
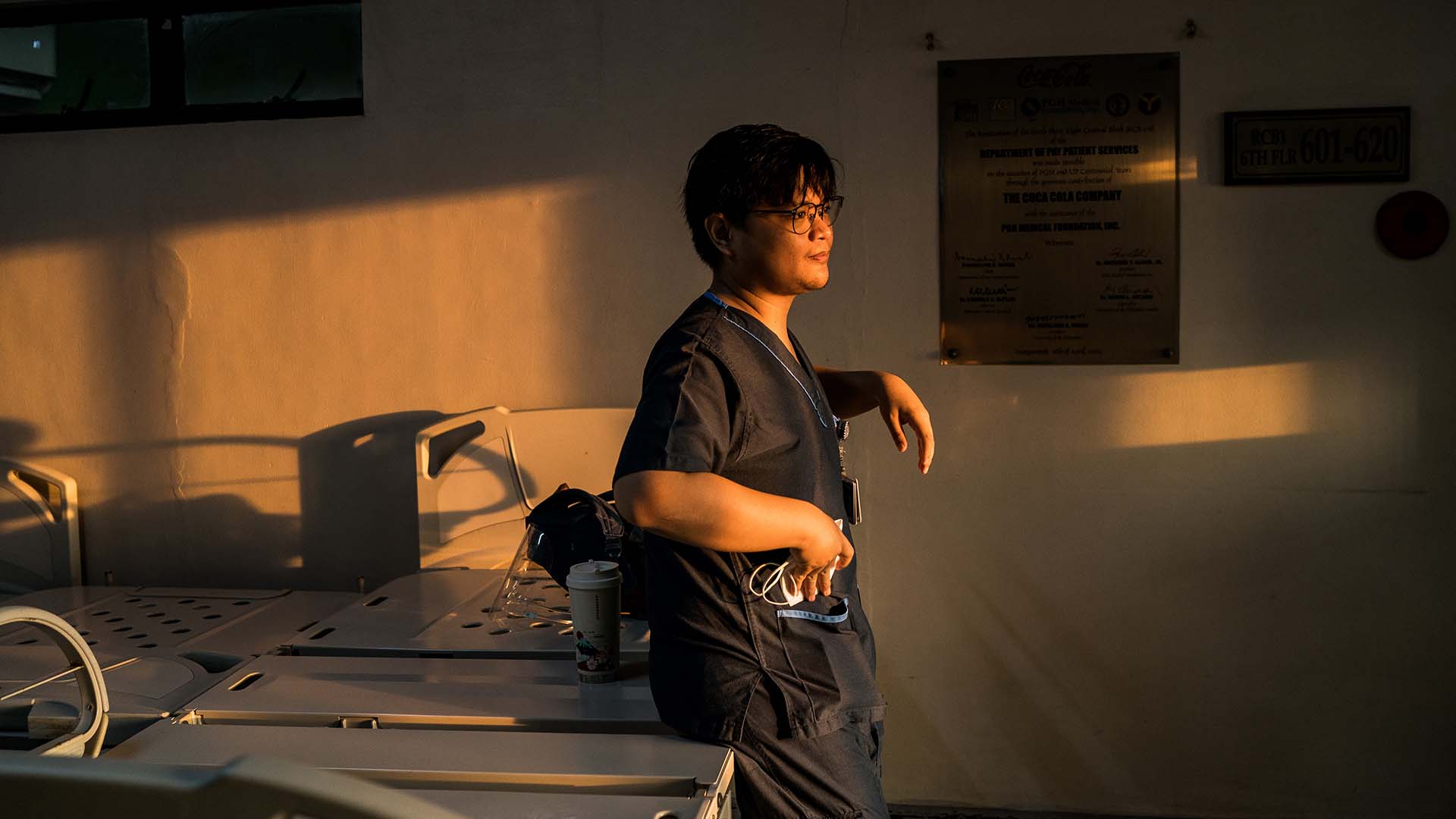
Frontline public healthcare provision in Brazil is conducted by community health agents (CHA) who act as a vital link between individuals and communities, especially those that are hard to reach. The Community Health Agent Programme forms a fundamental part of the country’s Programa Saúde da Família (Family Health Strategy), which relies on interdisciplinary healthcare teams that include a doctor, a nurse, a nurse assistant and up to six non-medical CHAs who are charged with providing universal access to public health and first-contact care.

Research has considered the impact of the pandemic on a wide range of medical staff, including nursing workers who are most intensively affected by the pandemic — presenting higher levels of anxiety, somatisation, dissociation, depression, hopelessness, acute stress and compassion fatigue. But such studies have not factored in CHAs, whose situation is less understood, in part because they are not formally considered to be healthcare professionals in Brazil.
This omission not only means that it is hard to provide an accurate assessment of the number of Brazilian CHAs who have experienced a downturn in their mental health during the pandemic, but also impacts any assessment of their wider health needs, not least because their deaths are not registered in Brazil's official statistics of healthcare worker mortality.

This reality leaves no room for interpretation. Systems-based and innovative solutions are needed to address these challenges in order to help frontline workers manage, prioritise and manage their wellbeing.
One such innovation comes in the form of an artificial intelligence (AI)-powered app, Vitalk, which is described by its developer as an “AI-powered virtual health assistant for primary care”. Vitalk currently provides support to more than 7,000 CHAs across Brazil, 68 per cent of whom self-identify as suffering from anxiety, 70 per cent from burnout, 51 per cent from depression and 71 per cent from low resilience.
The app is part of a new generation of mental health support and data collection technology that is being deployed through mobile devices to provide new ways to access help, monitor progress and increase the understanding of mental wellbeing.

Vitalk’s users can communicate with the app through a smartphone; if the AI behind the app identifies a problem that it cannot solve, it will guide its user to the most suitable health resource for their specific needs through Viki, the app’s virtual health assistant.
“I usually keep a reminder to use it twice a day. Once when I come home from work and then at 8pm. That is when I talk about how I am feeling and how my day went,” says 25-year-old Lucas Albuquerque, who works as a CHA in Bairro Vila Itaberaba, one of São Paulo’s northern neighbourhoods. “Since I have been using it for a while, Viki follows a chain of thought for the questions as I answer them.”

Before he became a CHA, Albuquerque sought the help of a psychotherapist in an attempt to prioritise his mental wellbeing, but he abandoned the treatment because of the demands of his job. Over the course of the last year, however, Vitalk has provided Albuquerque with a source of solace and guidance.
“I used to feel that I had to solve every problem, but I changed with time and discovered that I have a limit, otherwise I wouldn’t be able to handle it,” Albuquerque admits. “It has been especially stressful because there are many things we wish we could do, but we can only wait. This makes us feel powerless.”
Albuquerque says that one of the most important lessons he has learned from using Vitalk is not to wait until there is a serious problem before prioritising his mental health but rather to nurture it continuously, even when he is feeling well.

In many ways, Vitalk provides Albuquerque with the same ideas and strategies that he communicates to his own patients, the most important of which is the need to practise self-care. “We have so many reasons to be thankful. It can be for the air we breathe, food, water, simple things we have access to that some people do not,” he says. “We forget to be thankful, to be more positive, to take better care of ourselves, to try to pay better attention to people around us.”
As the authors of a recent paper have argued, the mental health and wellbeing of healthcare workers needs to be understood as an urgent global public health priority, and acted upon as such, through longer-term measures that are designed to effect systemic change.
“World leaders and other decision-makers need to fully realise the crucial importance and value of investing in the mental health and wellbeing of the healthcare workforce, on an individual, organisational and societal level,” they write. “Let us learn from our past and thank our essential healthcare workers by demanding and promoting real reforms within our healthcare systems. We cannot afford the cost of failing in this aim.”